Founded to create simple solutions to address gaps in health care, Ariadne Labs broadened its lens to create system-level change.
By Erin Lawler and Stephanie Schorow
Medical care can save lives. It can also harm them.
Nearly half of adverse medical events are associated with surgical operations; each year, seven million people are left dead or disabled due to surgical complications that we already know how to avoid. Patients living with serious illness undergo invasive tests and treatments that offer little benefit and take away from their quality of life. People giving birth and their infants face serious complications, and even death, from preventable causes.
Even before Ariadne Labs was founded, researchers were working in each of these three areas to address these gaps between the medical knowledge on how to do better, and clinicians’ ability to do it. Ariadne Labs set out to produce and promote use of simple tools to tackle challenges in health care.
While each of these programs began with a single solution aimed at a specific problem, all have since widened their lenses, and their impact, to address gaps across entire systems of care. “The simplicity of our work comes from the design. What is a tractable solution that might actually make a difference? From there, we’ve come to understand the system lens that’s required to envelop these simpler solutions into a long-term series of improvements,” said Executive Director, Asaf Bitton.
Bill Berry, a surgeon, recalled the day he was approached by Gawande about working on a project for the World Health Organization to improve surgery globally. “I said had one condition. We have to commit that this won’t end up on some dusty shelf…we’re actually going to take this to the ground, and we’re going to commit ourselves to take it to the world.” Berry added, “I think Ariadne was actually born in that little conversation.”
Berry and Gawande didn’t set out with the idea of a checklist. “We wanted to improve the care of surgical patients around the globe ,” Berry recalled. “We didn’t even know how big the problems were or what problems we should concentrate on.” After a two year process of large collaborative meetings with experts, rapid cycle testing, and feedback from the field, a checklist went into a trial. The results were positive.
The WHO Surgical Safety Checklist is a 19-item list of prompts intended to prevent mistakes and improve teamwork and communication in the operating room. It has made a major impact in operating rooms throughout the world. Studies have shown the Checklist to be associated with reductions in complications and mortality, with one, published in the New England Journal of Medicine, showing nearly a 50% reduction in mortality. A 2021 report marking 10 years of progress of the Checklist noted that the tool has been implemented in six continents and adopted in more than 70% of operating rooms around the world. It has impacted the lives of millions.
This tool served as the launching point for Ariadne Labs’ Safe Surgery/Safe Systems Program; today, it is one piece of a multi-faceted approach to improving surgical systems. The program now includes areas such as surgical training and coaching, use of digital health technologies to aid surgical recovery, and patient safety when health systems expand or onboard new clinicians.
The BetterBirth Program followed a similar trajectory from simple solution to system change. The BetterBirth Program began with the initial goal of evaluating the effects of the WHO’s Safe Childbirth Checklist and supporting its implementation. The checklist is intended to support birth attendants in delivering essential childbirth practices proven to address the biggest complications women and babies face.
The landmark BetterBirth study, conducted in Uttar Pradesh, India, found that the checklist, combined with a peer-to-peer coaching, increased adherence to the checklist items, but outcomes did not change. This result highlighted that no one factor affected maternal mortality rates; rather changes across the entire ecosystem of maternal and newborn health care were needed to improve health and save lives. The BetterBirth team continues to study the impact of the Checklist, with more recent work finding that its use does positively affect outcomes for mothers and babies when implemented as a part of broader quality improvement initiatives that address other systemic challenges.
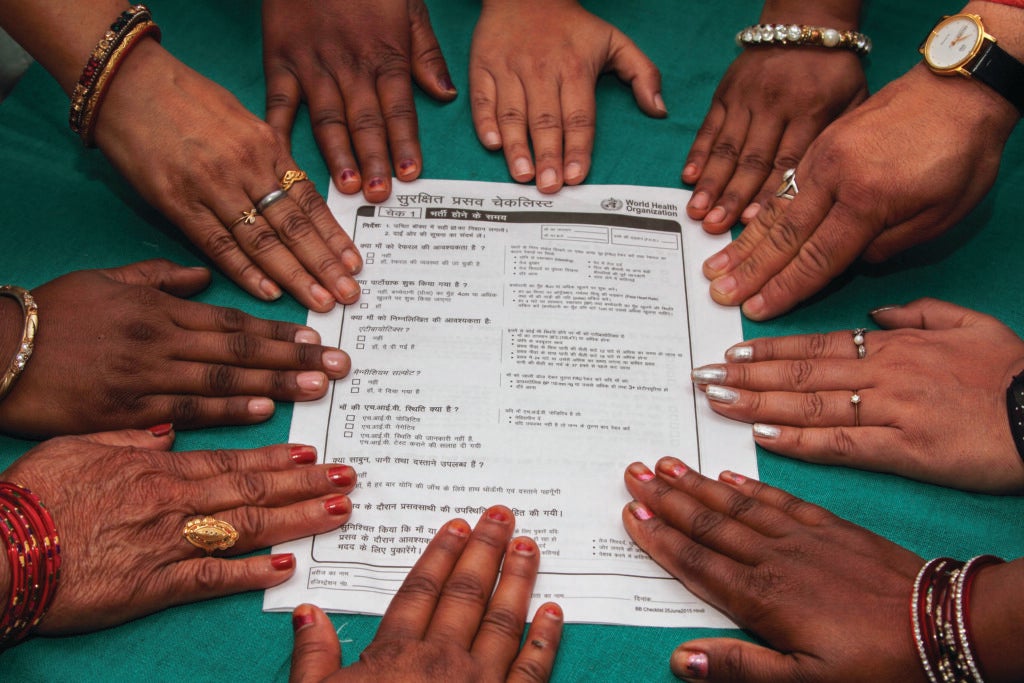
Katherine Semrau, PhD, MPH, who leads the program, was conscious that a checklist was only one aspect of improvement. She had previously volunteered on a trip to Honduras to aid in hurricane recovery and recalls recognizing that “Having doctors and nurses and pharmacists and dentists fly in from high-income countries…to try and patch things together, it’s not a solution. It was kind of like putting your finger in a dam that’s cracking and not really co-creating solutions or systems that need to be changed.”
Since that study, the BetterBirth team has expanded their portfolio of work to address issues of quality in private childbirth facilities and leads the Low Birthweight Infant Feeding Exploration study to understand current feeding practices for low birthweight infants and inform global feeding guidelines to help vulnerable infants survive and thrive.
Semrau said that BetterBirth projects have influenced policy decisions in India and even “how we define quality during childbirth.”
The Serious Illness Care Program has found that ensuring that patients’ goals and wishes are known and respected in their care is about a lot more than simply knowing what questions to ask. It requires creating a culture that values and enables those conversations throughout entire health care systems. Prior to Ariadne Labs’ founding, Susan Block, MD, had been leading a team of palliative care experts to develop and pilot a conversation-based intervention that improves care for patients with serious illness.
In 2012 Ariadne Labs’ Serious Illness Care Program began its flagship study at Dana-Farber Cancer Institute to test a system intervention that supports patient-clinician guided conversations about patient goals and values. The findings from the study trial suggested that the program reduced patient depression and anxiety by 50%, and led to more, better, and earlier conversations about what mattered most to patients in regard to their care.
Importantly, further research has shown that these outcomes are only achieved when the full program is implemented. For successful implementation, clinicians need to be trained on using the Serious Illness Conversation Guide, but system-level changes, including leadership engagement, electronic documentation systems, and program champions, are equally important.
“In ten years, we’ve learned a lot about what it takes to effectively and fully implement the conversation guide at a system-wide level, beyond individual clinicians,” said Stacey Downey, Associate Program Director. “We’ve put a lot of thought, time, and research into creating an implementation package with a structure and materials that gives systems what they need for uptake.”
To date, the program has reached more than 121,000 clinicians. The team has created a full implementation package to support systems in engaging leaders, changing practice, and measuring success to create a system that supports clinicians and patients before and beyond the moment of the conversation.
Lasting improvement hinges on system-level changes, and this realization would serve as a guiding principle for Ariadne’s continued growth.