Since its creation more than a decade ago, the WHO Surgical Safety Checklist has made surgery safer for patients around the world. However, simply displaying the Checklist in an operating room wall does not guarantee better outcomes. How the Checklist is implemented and ingrained into clinical culture plays a key role in its success.
A new paper in JAMA Surgery, published by members of Ariadne Labs’ Safe Surgery/Safe Systems with partners at Singapore General Hospital and Johnson & Johnson, highlights the importance of surgical teams regularly evaluating how the Checklist is performing in their operating rooms. Study findings show that by assessing and effectively reimplementing the Checklist, health systems can improve team behavior, safety culture, patient safety, and patient outcomes. The evaluation also allows teams to identify any gaps in the initial implementation process and to identify any revisions to the Checklist’s content to help it remain relevant as its context evolves.
The publication details work completed through a five-year partnership between Ariadne Labs’ Safe Surgery/Safe Systems Program, Johnson & Johnson, and SingHealth to evaluate and update Checklists at both Singapore General Hospital and National Heart Centre Singapore.
“Clinicians in Singapore recognized that preventable adverse events were occurring more often than they should be. Despite Singapore’s adoption of the Surgical Safety Checklist, these doctors and nurses determined that their Checklist was not being performed adequately,” said Mary Brindle, MD, MPH, Director of Ariadne Labs’ Safe Surgery/Safe Systems Program.
Brindle stressed that this experience is not uncommon, even among high-performance centers. “Singapore is a center with a track record of excellent care. They did not have more of an issue with this than any other place but were motivated to push their center to achieve even better outcomes,” she said.
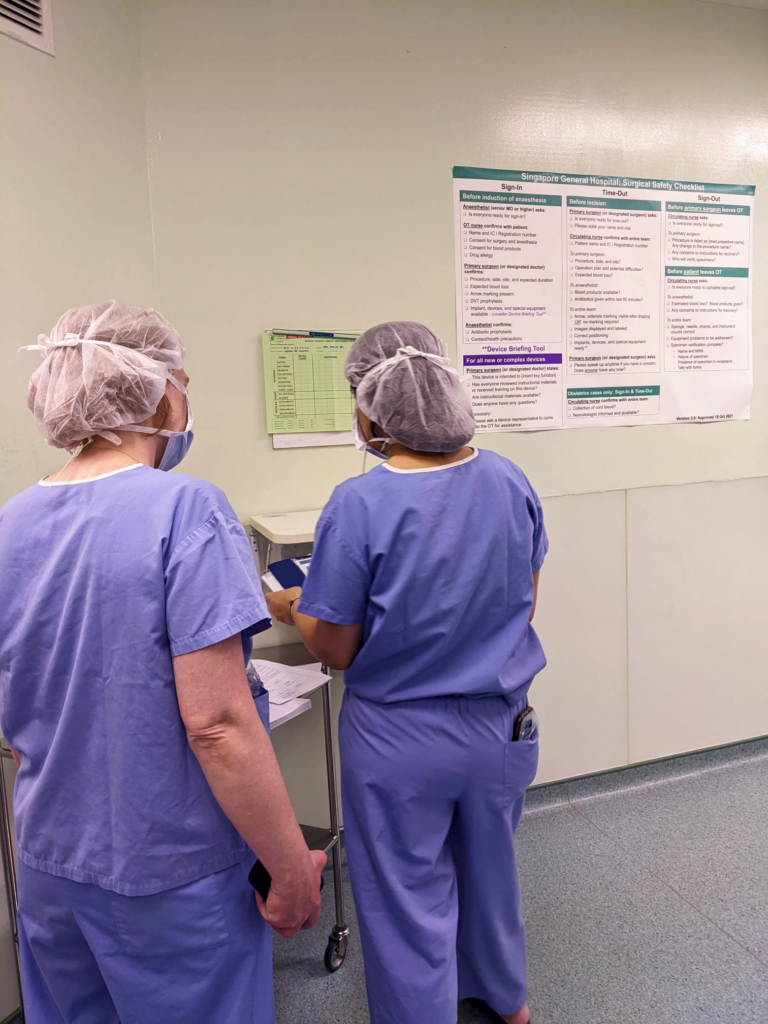
To address this gap, a team at Ariadne Labs worked with partners in Singapore to assess the quality of surgical care, safety culture, and Checklist performance at each facility. The team spoke with frontline stakeholders, sought recommendations for improvement, and identified surgeon and nurse champions to further bolster support for the Checklist. The team compared each institution’s version of the Checklist to the original WHO version and developed a “best-bet” model of the revised Checklist for pilot testing.
As part of the reimplementation process, the team also incorporated the Device Briefing Tool into the Checklist. This communication tool was developed in partnership with Johnson & Johnson to help surgical teams ensure accuracy when using new or complex devices, which have become increasingly common in operating rooms around the world. A paper published in Surgery showed that the tool was associated with a significant 28% reduction in device-related interruptions.
“Surgical device use accounts for almost 25% of errors during surgery; yet, the original Surgical Safety Checklist didn’t address those challenges,” said Rachel Moyal-Smith, DrPH, PA-C, Senior Clinical Implementation Specialist at Ariadne Labs. “By regularly evaluating and reimplementing their Checklists, surgical teams are able to incorporate new resources like the Device Briefing Tool to help them stay current with the ever-evolving risks and challenges they’re facing in the operating room.”
The revised Checklist was formally reimplemented in November 2021. The team hopes the findings from this paper will highlight the value of a formal evaluation and reimplementation process for other institutions whose Checklist may not be reaching its full impact.
“Ideally, all organizations would look at their Checklist performance, think about device safety, and see how they can integrate the Device Briefing Tool in an updated Checklist,” said Joaquim Havens, MD, Ariadne Labs faculty.
Learn more about this work in the below publications:
Device Briefing Tool and Device-Related Interruptions:
- Development and Feasibility Testing of a Device Briefing Tool and Training to Improve Patient Safety During Introduction of New Devices in Operating Rooms: Best Practices and Lessons Learned, Journal of Surgical Research
- Frequency of Device-Related Interruptions Using a Scalable Assessment Tool, The Joint Commission Journal on Quality and Patient Safety
- Utility of a Device Briefing Tool to Improve Surgical Safety, Journal of Surgical Research
- Implementation of a Device Briefing Tool reduces interruptions in surgery: A nonrandomized controlled pilot trial, Surgery
Checklist Evaluation and Reimplementation
- Creating a high-performance surgical safety checklist: A multimodal evaluation plan to reinvigorate the checklist, Journal of Evaluation in Clinical Practice
- Defining re-implementation, Implementation Science Communications
- CheckPOINT: a simple tool to measure Surgical Safety Checklist implementation fidelity, BMJ Quality & Safety
Non-Technical Skills Training
- Training Novice Raters to Assess Nontechnical Skills of Operating Room Teams, Journal of Surgical Education
- Virtual non-technical skills assessment training is an effective, scalable approach for novice raters, Journal of Surgical Education
- Non-technical skills in surgery during the COVID-19 pandemic: An observational study, International Journal of Surgery