Communication – whether between providers and patients, or among members of a care team – is critical to ensuring optimal care and patient safety. Our team has developed solutions to help collect data on surgical outcomes that matter most to patients to allow them to make informed decisions about their care. And, through our work to develop guidance for hospital expansion and physician onboarding, we aim to fill gaps in communication that often make it difficult for physicians working in new environments to quickly adapt. By tackling these challenges in communication, we work to ensure that patients have the information they need to make informed choices, and that the systems in which they receive care are ready to respond.
HealthPrism
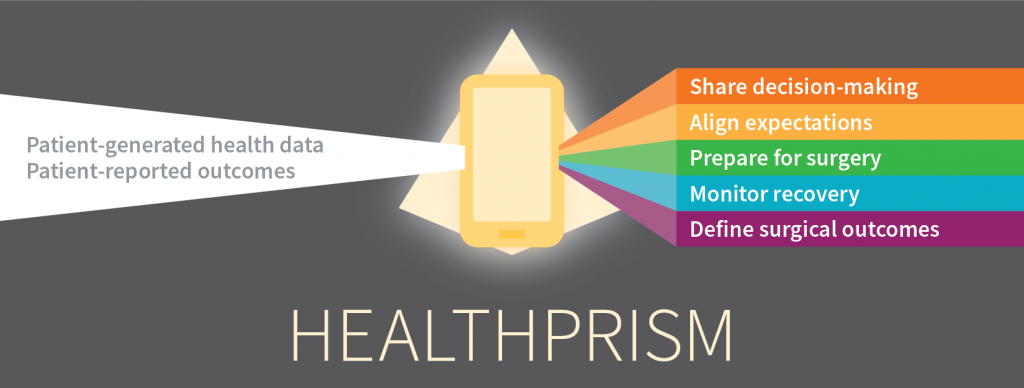
HealthPrism uses digital phenotyping, or moment-by-moment data collection from a person’s digital devices, to track their physical and mental health during post-surgical recovery.
Initially supported by an Ariadne Labs Spark Grant, the HealthPrism team recognized an information gap in surgical recovery. Often, clinicians do not capture the outcomes after surgery that matter most to patients, leaving patients to make difficult treatment decisions without an understanding of how their choices will impact their quality of life.
Without this information, patients continue to have high unmet information needs and misaligned treatment expectations, and may be inclined to undergo high-risk, low-benefit treatments.
HealthPrism captures data passively, such as through a smartphone’s GPS, and actively through brief surveys, audio recordings, and on-screen cognitive tests. Together, this information allows researchers to measure surgical recovery with data coming directly from patients on the outcomes that truly matter most to each and every patient.
HealthPrism is able to quantify surgical recovery by capturing nearly one billion interactions per patient each month, in addition to traditional patient-reported quality of life outcomes. This allows more informed shared decision-making around surgical care; improves patient-centered outcomes after surgery through early detection of stalled recovery; and develops a methodology to collect patient-centered outcomes on a large scale for surgical outcomes and comparative effectiveness research.
The HealthPrism team has collected GPS data from patient smartphones to determine differences in recovery after breast-conserving surgery as compared to mastectomy, and study how these data align with self-reported quality of life. The team has also used smartphone data to explore the impact of decision conflict on recovery in patients undergoing cancer-related surgery: patients who were conflicted or had second thoughts about their decision to undergo surgical treatment had lower levels of physical activity during their surgical recovery.
By continuing to gather patient-reported data on outcomes that matter to patients, HealthPrism can help provide patients with the information they need to make informed decisions about undergoing a surgical procedure.
Patient Safety for System Expansion
The expansion of health systems through mergers, acquisitions, and affiliations offers the opportunity to improve care for patients. However, without adequate planning and communication, it can also lead to unintended harm to patients. Ariadne Labs and CRICO/Risk Management Foundation partnered to develop a set of tools to guide health system leaders through a communication process that uncovers important patient safety considerations during major transitions.
The Patient Safety Discussion Toolkit for System Expansion is a manual for clinical leaders to use during the pre-affiliation. The toolkit:
- Guides clinical leaders on how to foster the right environment for these important discussions
- Offers recommendations on how to use the Discussion Guides
- Provides tips on how to turn the discussions into successful action plans
- Comes in four formats: Word, Excel, PowerPoint and PDF
The Discussion Guides provide a set of discussion questions to initiate conversations among clinical leaders about the patient safety risks that can be otherwise overlooked when systems merge. While the guides are ideally used during the pre-affiliation phase of system expansion, they can be employed at any time in the process to ensure critical safety issues are being addressed.
The All-Specialty Guide is to be used in all departments by all clinical leaders. Clinical leaders in obstetrics, surgery, and emergency medicine should supplement with specialty-specific guides. The guides:
- Encourage open lines of communication
- Foster relationship building and teamwork
- Uncover potential risks
- Support early planning to mitigate potential harms.
The Joint Clinical Integration Guide provides health system leaders with a set of guiding principles and action items for successful clinical integration that increases the value of care provided to patients. The guide is meant to be used once a system expansion agreement is in place.
The PSA Onboarding Tool is a guide of questions to make it easy for “traveling surgeons” to proactively identify differences in practices and resources between “home” and “away” care systems.
Rapid Onboarding Toolkit
Ariadne Labs has developed the Rapid Onboarding Toolkit for health systems to develop or strengthen their fast-paced onboarding process.
Clinicians who are rapidly redeployed to new roles or locations face challenges such as adapting to an unfamiliar setting and developing working relationships with new team members, often within a climate of fear and uncertainty. Intentional and efficient onboarding is crucial to ensure these clinicians are prepared to deliver safe and effective care.
The Rapid Onboarding toolkit includes:
- Rapid Onboarding Framework to assist the implementation leader(s) in structuring their onboarding program.
- Leader Implementation Guide which provides guidance to create an efficient and focused rapid onboarding program.
- Clinician Discussion Questions for frontline clinicians and redeployees to facilitate conversations with their team and manager to help prepare for their new role.
The toolkit was developed through an iterative design process which relied on two rounds of qualitative interviews with redeployed clinicians. Our goal was to identify key needs of clinicians who are rapidly onboarded to a new role and the most pertinent questions that would enable effective rapid onboarding for clinicians to safely care for patients and themselves.



