From leading global efforts to improve adaptation and implementation of the WHO Safe Childbirth Checklist to evaluating the impact of patient education and the quality of care in private childbirth facilities, the BetterBirth Program continues to innovate to close gaps in safety and quality in childbirth care.
Supporting WHO Safe Childbirth Checklist Implementation
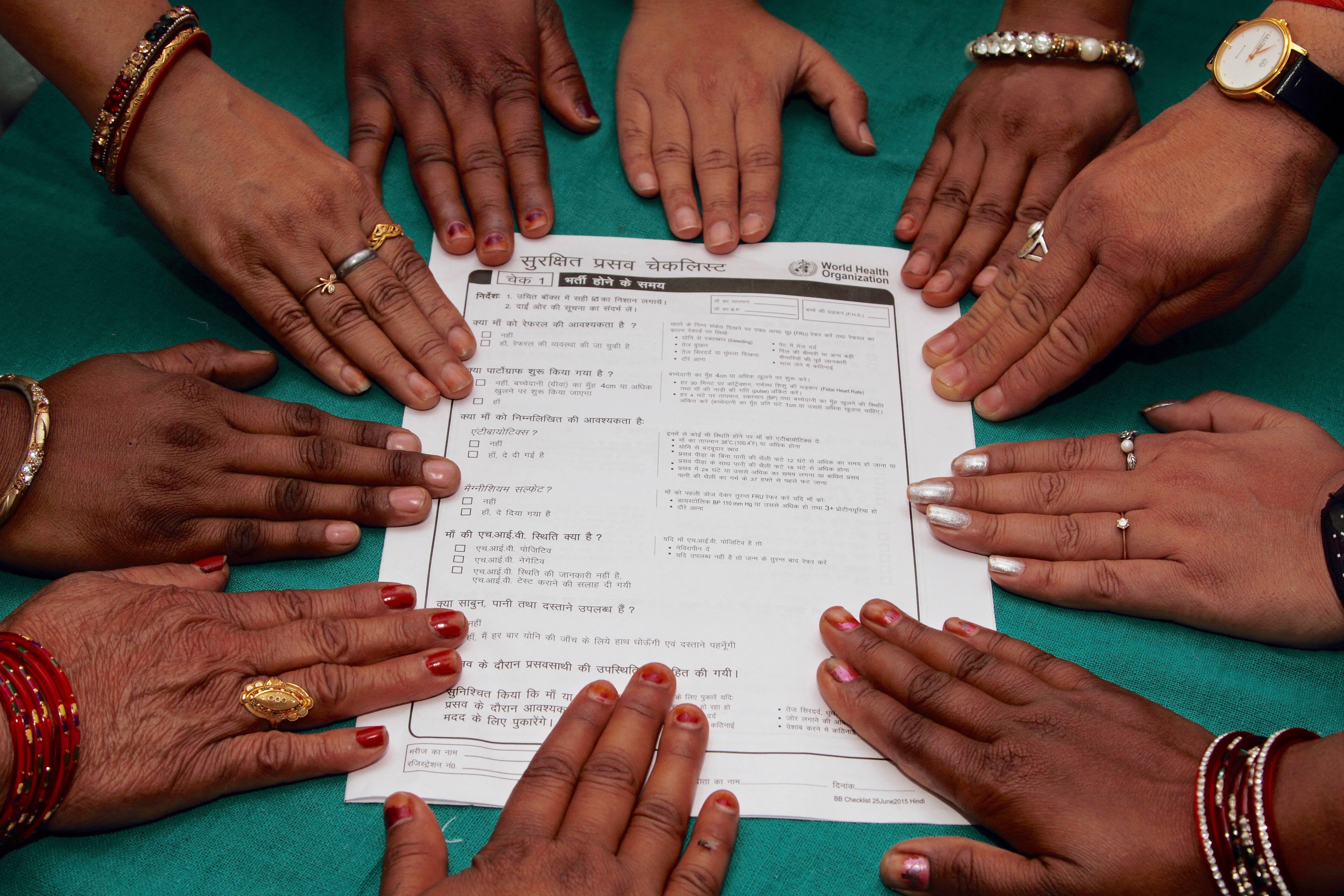
Since 2008, Ariadne Labs and the BetterBirth Program have played an integral role in the design, development, evaluation, and dissemination of the WHO Safe Childbirth Checklist and the accompanying implementation guide. Research from the BetterBirth Program and Checklist users around the world has highlighted the importance of adapting the Checklist and the implementation strategy to fit the local context. The BetterBirth team is leading efforts to identify best practices for adaptation and implementation to support users around the world.
The Checklist includes 28 essential childbirth practices to close gaps in safety and communication during childbirth. At least 35 countries have implemented the checklist worldwide, with an estimated 680,000 people impacted by the Checklist to date. In a number of countries, the Checklist has been incorporated into national policy and guidelines.
Community of Practice
To support implementation and adaptation of the Checklist around the world, the BetterBirth Program advocates globally for the use of the Checklist, supports users in implementing the Checklist in their contexts, and has created the Safe Childbirth Checklist Community of Practice. This online forum offers a place for Checklist users to share experiences, access implementation support resources, and learn from Checklist users around the world. The community is hosted on Ariadne Labs’ Aria platform.
The BetterBirth Study
From 2014 to 2017, the BetterBirth Program led the BetterBirth Study to test the coaching program for the WHO Safe Childbirth Checklist. The study highlighted that no single practice change can close gaps in safety and communication in childbirth care; rather, solutions are needed at the system level to close gaps across the entire ecosystem of care. Learn more about this trial in the landmark BetterBirth Report

FEATURED
The BetterBirth Study
This report synthesizes the learnings, findings, and insights from the Ariadne Labs BetterBirth Study.
SEE ALL RESOURCESIn 2021 the BetterBirth Program released an addendum to the report focused on management of complications at frontline facilities. The addendum includes an in-depth look at data from the BetterBirth Study on five life-saving, facility-based interventions: Referral, cesarean deliveries, antibiotic use, neonatal resuscitation, and oxytocin administration.
The BetterBirth Study provided a rich dataset that has been the basis of more than 20 peer-reviewed articles by the BetterBirth Program exploring health care worker behavior change, the link between behavior change and health outcomes, overuse of oxytocin, and more. See all research from the BetterBirth Program here.
The BetterBirth Program continues to identify new opportunities to close gaps in childbirth care. Other implementers around the world have published approximately 50 articles on Checklist use and related topics, such as mortality and morbidity outcomes, behavior change, respectful maternity care, integration with technology, Checklist adaptation/modification and validation, and Checklist implementation pathways.
Featured Research

Commentary from the BetterBirth team published in Lancet Global Health on how the Checklist is most effective when implemented as part of a larger quality improvement initiative and calls for more research.
LEARN MORE
A paper in NEJM led by the BetterBirth team looks at the effects of a coaching-based WHO Safe Childbirth Checklist Program in India on adherence to essential birth practices.
LEARN MOREPreventing Newborn Illness and Death through Family Education
In an ongoing study initiated in 2018, the BetterBirth Program collaborates with Noora Health to evaluate the impact of Noora Health’s maternal and neonatal Care Companion Program (CCP) on closing safety gaps in newborn care. In use at more than 100 hospitals throughout India, the CCP aims to educate new parents on critical preventive health practices for newborns with the goal of avoiding preventable newborn deaths. The study includes 24 sites throughout the country, reaching 90,000 patients.
Approximately 2.5 million newborns die each year within the first month of life, mostly in low- to middle-income countries. Many of these deaths could be avoided by educating families on practices such as keeping babies warm, breastfeeding, handwashing, and umbilical cord care; however a 2020 survey of more than 13,000 mothers in India led by BetterBirth and Noora Health found significant gaps in such education. Less than 50% of the mothers surveyed had received education on newborn care before leaving the hospital. Only 25% of respondents recalled being taught about breastfeeding, and fewer than 10% recalled being taught about hand hygiene, umbilical cord care, or warning signs of newborn illness. These results indicate there is a clear opportunity through programs such as the CCP to improve education strategies, empower providers, and support families.
By evaluating the CCP, BetterBirth and Noora Health aim to assess the program’s impact and identify opportunities for adaptation in advance of program expansion in India.
Early results from the study have found positive impacts on parent knowledge and behaviors. Final results on the CCP’s impact on improving knowledge, behavior, and health outcomes are expected in 2022.
Featured Research

Members of Ariadne Labs’ BetterBirth team and Noora Health discuss the importance of educating new mothers and their families in India, especially during the COVID-19 pandemic.
LEARN MORE
A paper in BMJ Global Health, written with input from Ariadne Labs’ BetterBirth researchers, looks at how postnatal education may help families survive and thrive.
LEARN MOREPartners

Measuring Quality in Private Sector Facilities in India
The BetterBirth team partners with Manyata, a childbirth quality improvement and certification program in India, to study the program’s impact on improving the quality of childbirth care in private facilities to close gaps in safety and integration.
In India, 36.8% of institutional deliveries occur at private sector facilities; however, these facilities often are not regulated, and quality monitoring is limited. There is a general consensus amongst the public that private sector facilities offer higher quality care, yet data to support that sentiment is lacking.
Manyata was developed based on the WHO Safe Childbirth Checklist. It aims to improve the quality of care at India’s private sector childbirth facilities by assessing facilities’ performance on 16 key clinical quality standards, such as antenatal care, prevention of postpartum hemorrhage, and adherence to infection and complication protocols.
The BetterBirth Program is assessing what makes Manyata valuable to those participating in it, what practices within facilities Manyata was effective in changing, what ones are more difficult to change, and what types of facilities are most successful with the program. The findings of the evaluation will be used to inform the next stage of the Manyata program, which has the goal of scaling to 10,000 facilities across India.
Implementation of Manyata is supported by Jhpiego and the Federation of Obstetrics and Gynecology of India.