By June-Ho Kim, Jessica Wiken, and Joey Ross
Countries around the world are driving towards universal health coverage by 2030. There is growing consensus that high-quality health coverage must be supported by strong primary health care (PHC) systems. However, many PHC systems are not capacitated with the governance, policy, and finance levers needed to be effective and achieve this vision of high-quality services for all.
The Primary Health Care Performance Initiative seeks to engage with low and middle income countries to measure PHC system characteristics, services, and outcomes to inform and guide improvement efforts. Ariadne Labs is leading the Initiative’s efforts to develop new approaches to filling pervasive measurement gaps so clearer pictures emerge in our collective understanding of how countries’ health systems operate and where barriers exist to the implementation of high-quality PHC at the local level.
In particular, we found few measures around person-centeredness and facility management capacity — key elements for improving equitable service delivery and ensuring that facilities are able to comprehensively respond to a person’s needs. These gaps underscored the need for rapid and high-quality data collection that supports the use of person-centered measures.
To fill this critical gap in measuring PHC effectiveness, the Primary Health Care team at Ariadne embarked on a partnership in 2016 with the Bill & Melinda Gates Institute for Population and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health (JHSPH) and the Kwame Nkrumah University of Science and Technology (KNUST) to design and conduct national surveys of patient experience and facility management in primary health care in Ghana.
The survey was built on the innovative Performance Monitoring and Accountability 2020 (PMA2020) mobile survey platform and yielded insights into the impact of facility management on patient experience, among several other findings. The partnership between Ariadne Labs, JHSPH, and KNUST was highly effective because of the collaborative approach and KNUST’s extensive experience engaging the PMA platform in the local context. The experience created a productive template for integrating new PHC measurement indicators into an existing survey platform.
National Primary Health Care Survey Implementation in Uganda
Building off of the successful partnership with the PMA2020 platform and network in Ghana, the team collaborated with JHSPH and the Makerere University School of Public Health (MUSPH) to deploy a national survey of PHC in Uganda. Our collective vision was to rapidly and accurately assess the current performance of Ugandan PHC facilities and Ugandans’ experience of care. In February 2019, members of Ariadne Labs and MUSPH teams convened in Kampala, Uganda’s capital city, to train 110 survey enumerators and 20 supervisors on the concepts and questions behind the PHC assessment. Fielding of the survey kicked-off in March, and garnered national Ugandan media coverage.
Over the next three months, enumerators spread out across the country and surveyed nearly 5,000 individuals and 400 health facilities, collecting survey responses and GPS data using Android smartphone devices. Data were immediately uploaded into a cloud server monitored by the MUSPH and JHSPH teams. By June 2019, teams had completed the data cleaning and quality checks. We were able to initiate our first round of analyses and glean insights that could be rapidly disseminated to policymakers, health system leaders, and patient advocates.
The national survey provided insights into the care-seeking behaviors of both men and women in Uganda as well as into the barriers to seeking timely and effective care. We found that over two-thirds of the Ugandan population had sought care in the six months before the interview, mostly for acute problems such as fever rather than care for prevention or chronic illnesses. Of those who sought care, 40% did not go to their nearest health facility — many because that facility did not provide the right services or was too expensive. Of those who did not seek care and were presumed to be sick, most noted geographic barriers to accessing care.
Disseminating Findings with National and Regional Stakeholders
In October 2019, just seven months after the first interviews began, the MUSPH, JHSPH, and Ariadne Labs teams convened national and regional dissemination events in Uganda to review and discuss the survey findings and implications. The timing of the dissemination coincided with global policy dialogues that helped elevate the visibility of the findings — the U.N. General Assembly had met the week before to emphasize PHC as a foundation for universal health care. Over 100 people, ranging from members of parliament and officials from the Ministry of Health to consumer advocacy organizations and the media, attended the national event.
Survey findings focused attention on the Ugandan government’s current debate of a bill proposing a National Health Insurance Scheme to provide universal health coverage to all Ugandans. Data from the PHC survey showed that 99% of the population reported not having any health insurance, and 44% of those who sought care had to borrow money or sell possessions in order to afford the cost. Financial barriers to access were even more apparent in the rural areas.
These issues set the stage for a dynamic panel discussion during the event. The panel included Mr. Moses Kirigwajjo (Uganda National Health Consumers’ Organisation), Dr. Martin Ssendyona (principal medical officer from the Ugandan Ministry of Health), Honorable Baguma Spellanza (vice-chairperson of the health committee from the Ugandan Parliament), and Dr. Ivan Kamya (Head of the Ugandan District Health Officers). There was consensus that PHC in Uganda required additional funding and resources, particularly at the local level, and that there was a need to expand the health care workforce. Additionally, panelists emphasized that care should be comprehensive to include chronic conditions.
In a closing statement, Dr. Joseph Okware, commissioner at the Ministry of Health, noted that PHC is under-emphasized, under-measured, and under-funded. He called for the implementation of the National Health Insurance Scheme to support PHC and universal health care.
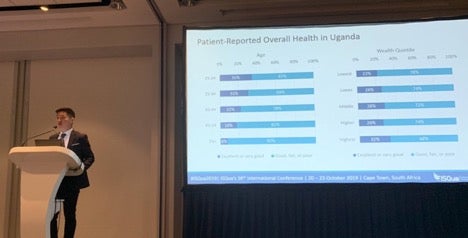
Sharing Lessons from Person-Centered Measurement in Sub-Saharan Africa
The PMA2020 PHC surveys in Ghana and Uganda represent an innovative integration of patient-reported outcomes and experiences into national PHC assessments in sub-Saharan Africa. In October of 2019, the Ariadne Labs team was invited to present on the implementation process and lessons learned at the 36th International Conference of the International Society of Quality in Healthcare (ISQua) in Cape Town, South Africa. In particular, the audience was interested in the PMA2020 team’s methodology. Using mobile technology and a broad network of survey enumerators who had trusting relationships with participants, the team was able to complete a nationally-representative survey in low-resource settings with rapid turnaround, outstanding response rates (>90%), and novel policy-relevant insights.
Next Steps
Through the research and development work of the Ariadne Labs PHC team, we seek to build partnerships similar to the PMA2020 surveys in Ghana and Uganda to fill data gaps and accelerate PHC data analytics towards advancing health systems globally. We believe that through close collaboration, data sharing, and innovation in measurement and dissemination, we can reach our vision of learning health systems that transform the global state of primary health care.