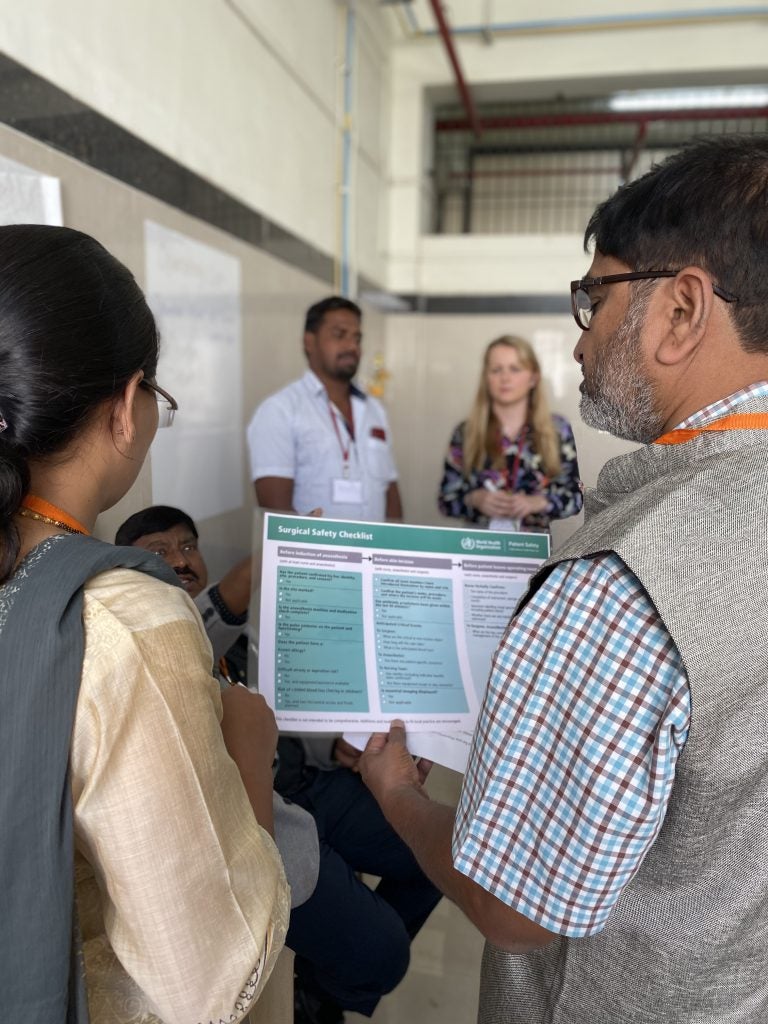
Ten years ago, a publication in The New England Journal of Medicine introduced the World Health Organization’s Surgical Safety Checklist. With that publication began a new movement in surgical safety around the world.
Over the past year, Ariadne Labs partnered with Lifebox, the global surgical safety non-profit, to develop an in-depth report on the impact of the 19-item WHO Surgical Safety Checklist since that seminal publication. Researched and written by Marine Buissonniere, Checking in on the Checklist uses interviews with implementers, peer-reviewed research, and extensive data analysis to present insights on global uptake of the Checklist, challenges to its implementation in different contexts, and opportunities for successful scaling of the tool, exploring a path forward for the next 10 years.
A decade after its launch, facilities in 70% of the world’s countries attest to using the Checklist, according to the report. While not all studies have shown significant impact on clinical outcomes, others have shown that Checklist implementation is associated with a reduction in surgical deaths of up to 36%. And beyond its clinical effects, users say the Checklist has been instrumental in introducing a culture of safety, improving communication, strengthening efficiency, increasing trust, and empowering practitioners.
“Over the last 10 years, the Checklist has gained incredible traction and has played a direct role in making surgery safer for patients around the world,” said Asaf Bitton, MD, MPH, Executive Director of Ariadne Labs. “But we’re not done. Our goal for this joint report with Lifebox is to offer a roadmap for further progress to ensure that the impact of the Checklist continues to grow and eventually reaches every surgical patient worldwide.”
A 2020 study by Delisle, et al looks back at the last 10 years to determine the global uptake of the checklist. The paper concluded that across nearly 1,500 facilities in 94 countries, the Checklist was used on average, in 75% of surgical interventions, confirming that uptake is generally high.
Despite the impact of the Checklist, the 2020 study also highlighted key gaps in use, particularly among countries with Low Human Development Indexes — a country-level measure of health, education, and standard of living — where the checklist was used in only about one-third of operations. Checklist use was also lower in less complex surgeries, in certain specialty areas such as obstetrics and gynecology, and in emergency surgeries.
“The uptake of such a simple and effective tool as the Surgical Safety Checklist around the world in less than 10 years is nothing less than a global health success story that is having a truly positive impact on patient lives around the world every day,” said Kris Torgeson, Global CEO of Lifebox. “We were excited to work with Ariadne Labs on this report showing the critical importance of further implementation progress so that all patients reap the benefits of safer surgical practice.”
The task now at hand is to further the systematic use of the Checklist to make surgery safer for every patient around the world. Checking in on the Checklist provides a qualitative look at the work that remains to be done to successfully scale the Checklist in a variety of settings and contexts.
The report additionally explores barriers to Checklist uptake that implementers have encountered over the last ten years, ranging from entrenched hierarchy in the operating room, to a lack of adaptation to local contexts, to the perceived amount of time or work required to complete the Checklist. Each barrier represents an opportunity to continue to improve checklist uptake over the next decade.
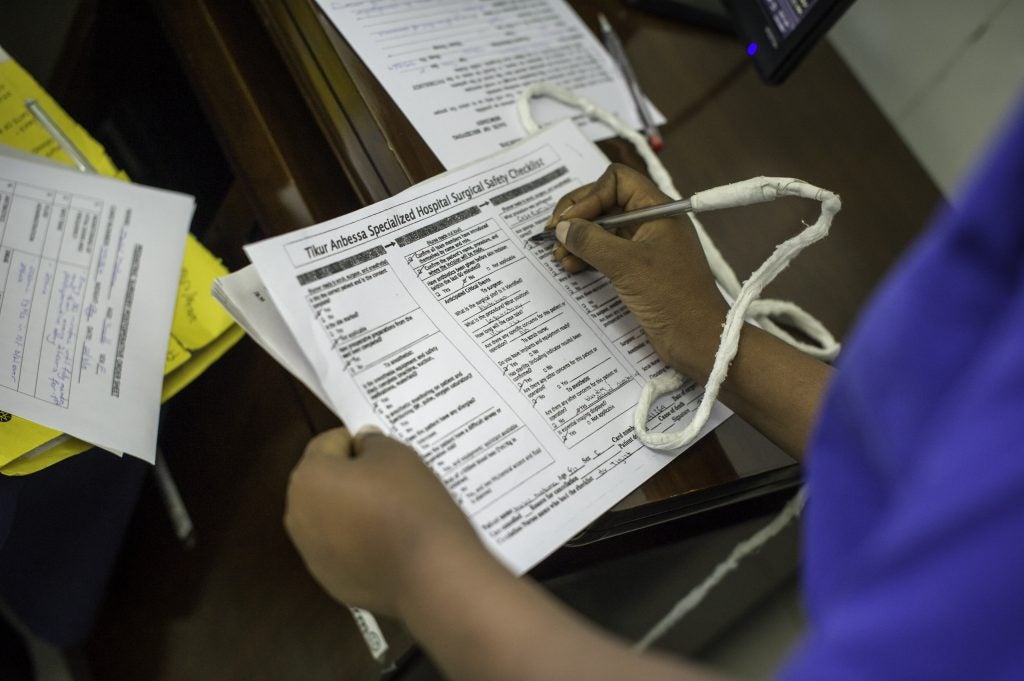
Beyond perceptions of the Checklist itself, context plays an important role in implementation. For example, in hospitals with strong political, socioeconomic, and technical foundations, the Checklist serves as a “safety net” — a reminder of the things that should be done. In resource-constrained settings, however, the Checklist may highlight key practices in surgical processes that must be improved before Checklist items can be completed safely. Strategies to support implementation in these settings will be a critical focus of implementation efforts over the next decade.
While barriers remain, ten years of studying Checklist adoption have also shed insights on the key factors that lead to successful implementation and sustained use of the Checklist. The report boils these recommendations down into three key categories:
Buy-in: Engaging all relevant practitioners and stakeholders to secure leadership support, address any concerns, and develop partnerships between local leadership and health officials.
Adaptation: Tailor and adapt the checklist to local contexts, including adding, removing or modifying Checklist items, redistributing responsibilities to align with staff practices, and translating items to the local language.
Accountability and Support: Balancing top down mandates with bottom up implementation approaches, using a combination of policy change and individual champions to create lasting change.
The last decade has shown that the Checklist has an important role in making surgery safer for patients. It has also revealed further questions and challenges to be addressed in the Checklist’s second decade. The report provides additional context into opportunities for successful scaling of the tool across all settings, and offers additional insights learned from implementers over the last ten years to guide the Checklist into the next decade.
Atul Gawande, MD, MPH, surgeon and writer who, together with clinicians and global health professionals, launched the Checklist, reflected on the progress of the last 10 years, saying, “There’s no single remedy to ensure safe surgery for all, but a simple, low-cost, high-impact tool like the Checklist helps make sure every person can get the right care everywhere, every time.”



