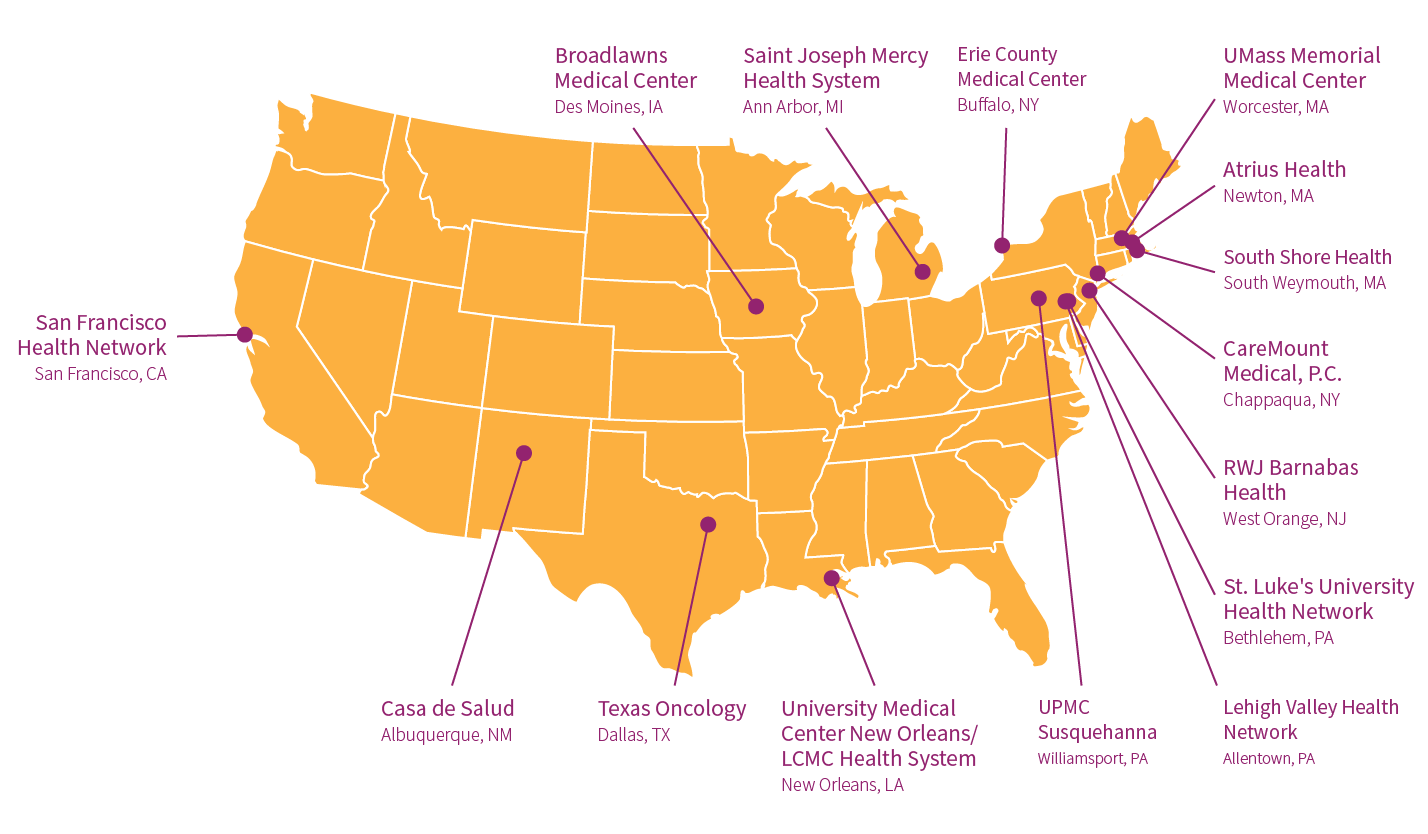
In June of 2019, Ariadne Labs launched the second, year-long phase of its Serious Illness Implementation Collaborative – a training and support program for health systems implementing the Serious Illness Care Program. The program promotes more, earlier, and better conversations among patients and clinicians about patient priorities, goals, and values for care when facing a serious illness. The collaborative first launched in September 2018 with a cohort of seven health systems, and expanded to include an additional 15 health systems across the US in its second phase.
“The collaborative members are real innovators and leaders – building their health systems’ capacity to ensure that patients feel heard and cared for on their own terms,” said Erik Fromme, MD, faculty on the Serious Illness Care Program. “Through the collaborative, we aim to provide them with the tools, training, and implementation support needed to act as champions of the program within their own systems.”

Over the course of the program, Ariadne staff provided collaborative members with one-on-one coaching calls and over 48 hours of group trainings, including webinars, learning groups, and an in-person training in September. When COVID-19 derailed plans for an additional in-person training, staff quickly pivoted to successful virtual trainings this spring. Trainings provide participants with the skills needed to train clinicians within their own systems on how to conduct effective serious illness conversations, as well as skills in gaining institutional buy-in for the program and communicating about the importance of these conversations. Members also received access to Ariadne’s digital implementation support platform, Aria.
During a recent, collaborative-wide celebration to mark the end of implementation effort, a collaborative member from Erie County Medical Center shared how, since first beginning to use the Serious Illness Conversation Guide in 2016, their organization had successfully trained hundreds of clinicians on using the guide. However, they decided to join the collaborative to help integrate the program at a system level. “We have moved a little further along…we’re seeing how this can be actual systems change, which is tremendous.”
In the collaborative’s second phase, more than 240 clinicians across the participating health systems were newly trained on conducting effective serious illness conversations with patients, significantly expanding the number of patients benefiting from important discussions around what matters most to them as they consider the best course of treatment for their illness.
“What’s really exciting is the incredible diversity of the health systems and their different approach to implementation, from a free-standing clinic serving a primarily Spanish-speaking community in New Mexico to a multi-hospital integrated health system in New Jersey,” said Fromme. “No matter where you are or who you are, having a health care team that understands what is important to you – and is prepared to have that conversation with you – is a critical part of high-quality serious illness care.”
Collaborative participants had an opportunity to reflect on their major successes, roadblocks, and visions for the future of the Serious Illness Care Program in their health systems.
Many shared how, despite delays and training limitations due to COVID-19, they were able to make significant progress in acclimating key stakeholders within their health systems to using the Serious Illness Conversation Guide. One collaborative member from Broadlawns Medical Care said, “We were surprised to see how open our clinicians were, and we think it’s owed to the fact that the guide makes so much sense, and there’s research and data to show how well it works. It lends to really good buy-in.”
Members also noted that since implementing the program, clinicians have viewed the conversations as more manageable and “doable in their day-to-day practice.”
As COVID-19 emerged, many systems faced shifting priorities and added barriers to implementation. However, for some systems, the pandemic helped highlight just how important it was for clinicians to receive training in speaking to patients about their priorities for care. Collaborative members spoke of the ways in which they adapted to ensure this important work continued, including developing virtual trainings for clinicians.
Each of the 15 systems is now looking to the future of their implementation and hope to continue to grow the program within their system. Members laid out goals focused on training more clinicians and expanding access, and committing at a system level to improve patient care through more, earlier, and better serious illness conversations. As a collaborative member from UMass Memorial Health Center said, systems are striving to ensure that the program becomes a part of “the DNA of our system.”