Maternal-newborn health leaders agree: after decades of significant global progress, it is possible to drive the changes that will be needed to finally end the preventable deaths of women and newborns in childbirth worldwide.
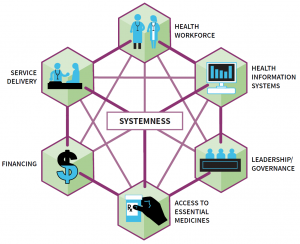
A new Ariadne Labs report launched at betterbirth.ariadnelabs.org aims to support the global effort with unprecedented data and evidence about what is happening at the frontline of childbirth care. The report’s key recommendation: focus on building “systemness,” or integrated, cohesive, and seamless care for women and their newborns.
The report, “The BetterBirth Study: Global Strategies to End the Preventable Deaths of Women & Newborns in Childbirth” made its international debut at the Women Deliver Conference held in June in Vancouver, Canada. It synthesizes the learnings, findings, and insights from the BetterBirth Study, one of the world’s largest studies of maternal-newborn quality of care and mortality. In addition, the BetterBirth team culled learnings and insights from members of the World Health Organization’s (WHO) Safe Childbirth Checklist Collaborative, representing sites around the world adapting and implementing the checklist. The report concludes with global recommendations and strategies for policy makers, program designers, implementers, and health system leaders.
“The message of the BetterBirth Report is that change is possible, and we still have work to do,” says Ariadne’s BetterBirth Director Dr. Katherine Semrau, an epidemiologist and maternal-newborn health expert. “What we found is that the solution does not lie in any single clinical practice or health system input, but rather the cohesiveness of the whole system. I’m looking forward to opening a global dialogue around systemness as a new lens for improving care and solving preventable maternal-neonatal mortality.”
The 2014-17 BetterBirth Study evaluated the impact of the BetterBirth intervention, combining the WHO Safe Childbirth Checklist with peer-to-peer coaching for birth attendants and data feedback. Overall, the program drove significant improvement in the quality of care delivered, but did not reduce maternal-newborn mortality. Those study findings were reported in 2017 in the New England Journal of Medicine.
Next, Ariadne researchers went back to the data. They spent more than a year analyzing 204 million data points from more than 157,000 women participants and their newborns to better understand what is happening at the frontline of care. That analysis comprises the new report. The learnings are organized around the four levels of the childbirth ecosystem:
- Birth Attendant: Competency and Workplace Matters
- Frontline Childbirth Facility: Readiness Matters
- Health System: Systemness Matters
- Women and Community: Power Matters
The report concludes, “The BetterBirth Study, along with other programs around the globe that have implemented the WHO Safe Childbirth Checklist, has shown change is possible in improving quality of care during the moment of childbirth. But sustained transformation in the way women and newborns are cared for before, during, and after birth will require an ambitious, dedicated, multifaceted effort.
Incremental improvements in the building blocks of a health-care system—workforce, service delivery, medical information databases, access to essential medications, leadership and governance, and financing—are critical. But they are not enough.
Reducing maternal and neonatal deaths will require a comprehensive approach that addresses system complexity around childbirth.”
For additional findings from the BetterBirth Report, visit our BetterBirth Study site.