WHO Surgical Safety Checklist
SAFE SURGERY CHECKLIST TEMPLATE
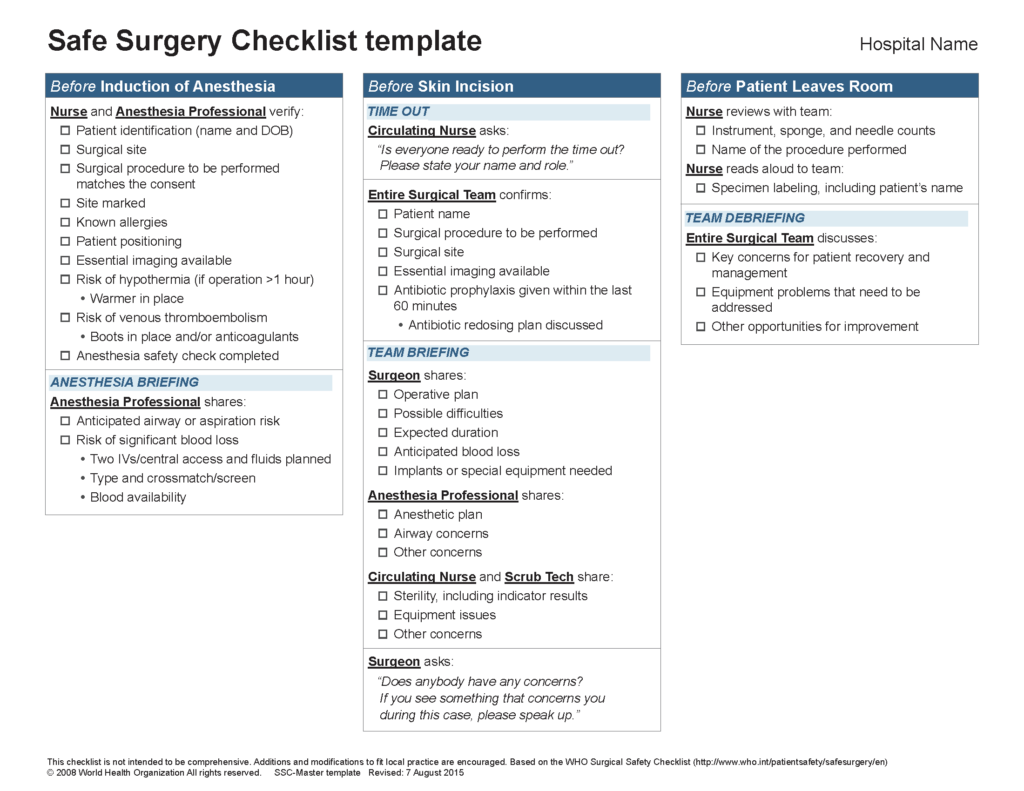
This checklist template is designed for all three sections (Before induction of anesthesia, before skin incision, and before patient leaves the room) to be performed in the operating room. This checklist doesn’t preclude or change any of the existing routines you have in your preoperative area.
The World Health Organization (WHO) Surgical Safety Checklist aims to improve surgical outcomes by outlining a series of steps taken before, during, and after a procedure to ensure surgical teams follow all safety protocols. In 2008, the WHO adopted the Surgical Safety Checklist as the global standard of care, and the Checklist became a core program of Ariadne Labs in 2012.
The Checklist identifies three critical pause points for surgery:
- Before the induction of anesthesia,
- Before the incision in the skin, and
- Before the patient leaves the operating room.
At each pause point, the Checklist encourages preparation, communication, and adherence to important practices that reduce errors and help surgical teams work together. By using the Checklist to build effective communication and teamwork, surgical teams can minimize the most common and avoidable risks.
Ariadne Labs collaborates with hospitals and medical facilities around the world to implement, evaluate, and adapt the Checklist.
Studies have been conducted around the world to understand the effects of the checklist on surgical safety, with most findings pointing to a positive impact. For example, in the first study of country-level impact of the Checklist, Scotland saw a 36.6 percent reduction in post-surgical deaths since implementing the Checklist as part of a national health safety program.
Uptake of the Checklist has been widespread. A 2020 report on the first decade of the WHO Surgical Safety Checklist, Checking In On the Checklist, found that facilities in 70% of the world’s countries attest to using it, though more work remains to disseminate the Checklist in diverse settings. Beyond its clinical effects, users say the Checklist has been instrumental in introducing a culture of safety, improving communication, strengthening efficiency, increasing trust, and empowering practitioners.



