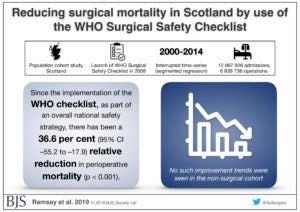
 In the first study of country-level impact of the WHO Surgical Safety Checklist, Scotland saw a 36.6 percent reduction in post-surgical deaths since implementing the checklist as part of a national health safety program.
In the first study of country-level impact of the WHO Surgical Safety Checklist, Scotland saw a 36.6 percent reduction in post-surgical deaths since implementing the checklist as part of a national health safety program.
The findings, reported in the April 17 British Journal of Surgery, are based on an analysis of 6.8 million operations performed between 2000 and 2014. The Surgical Safety Checklist was introduced in Scotland in 2008 as part of the Scottish Patient Safety Programme, and by 2014 the rate had decreased by 36.6 percent over six years to 0.46 deaths per 100 procedures. Researchers noted that this fall in death rates was not seen in patients who did not have surgery.
“This is a significant study which highlights the reduction in surgical mortality over the last decade. While there are a number of factors that have contributed to this, it is clear from the research that the introduction of the WHO’s Surgical Safety Checklist in 2008 has played a key role,” said Jason Leitch, Scotland’s National Clinical Director.
“This decline in mortality has been achieved through the hard work of hundreds of people involved in the project across the NHS in Scotland, delivered under the Scottish Patient Safety Programme alongside a number of other surgical safety measures. Behind every one of these statistics is a life saved, demonstrating the impact that the Scottish Patient Safety Programme has had and continues to have on delivering safe, effective and person-centered healthcare for patients. I am delighted that this work, which has the support of Scotland’s Royal Colleges and surgical societies, has been recognized in this way.”
NHS Scotland implemented the checklist across the country as part of the Scottish Patient Safety Programme and in partnership with the Institute for Healthcare Improvement. This was done through a collaborative, multi-disciplinary model including clinician support, staff education, leadership training and continual data collection. Regular nationwide meetings were held to share effective implementation strategies.
Surgical leaders from Ariadne Labs served as advisors for the Scotland implementation.
“This study reaffirms the importance of the WHO Surgical Safety Checklist which functions as a key aide in promoting effective team working, communication and other relevant non-technical skills in surgery which is critical in ensuring good outcomes,” said co-author Dr. Manoj Kumar, surgeon and National Clinical Lead for the Scottish Mortality and Morbidity Review Programme.
“The successful reduction in surgical mortality is a testament to the commitment from every member of staff and the teams involved in the delivery of high-quality patient care in NHS Scotland. We are delighted to have had the opportunity to work with the pioneers of the WHO Surgical Safety Checklist and colleagues from Ariadne Labs to better understand the impact of the Surgical Checklist on patient outcomes in Scotland.”
“Scotland’s well-planned, collaborative approach to implementing the checklist demonstrates how a national quality improvement project for the OR can be successful,” said co-author Dr. Alex Haynes, a surgeon and director of the Safe Surgery Program at Ariadne Labs. “This study adds to the growing body of evidence we have about best practices for successful implementation of Surgical Safety Checklist at scale.”
The World Health Organization developed the Surgical Safety Checklist a decade ago with a team of experts led by Dr. Atul Gawande, founder of Ariadne Labs. The 19-item checklist is designed to promote a culture of operating room teamwork and communication that improves surgical care and safety. Over the years, the checklist has been widely implemented with different strategies in settings around the world. In 2017, hospitals in the state of South Carolina, USA, reported a 22 percent reduction in post-surgical death rates after introducing the Surgical Safety Checklist with a voluntary program implementation program.
Gawande, a study co-author, noted, “Scotland’s health system is to be congratulated for a multi-year effort that has produced some of the largest population-wide reductions in surgical deaths ever documented.”


