In our new series, we highlight the staff and faculty behind the compelling work at Ariadne Labs. Hannah Ratcliffe discusses how the Ariadne team is working to strengthen primary health care globally.
 After obtaining a degree in biology, Hannah Ratcliffe worked as a bench scientist but says she soon realized “the details of protein pathways just really didn’t excite me.” What did excite her were aspects of her job that touched on the global prevalence and human impact of disease. “I’m really passionate about women’s rights and women’s empowerment,” she says. “And so my entry into global health was around maternal health.”
After obtaining a degree in biology, Hannah Ratcliffe worked as a bench scientist but says she soon realized “the details of protein pathways just really didn’t excite me.” What did excite her were aspects of her job that touched on the global prevalence and human impact of disease. “I’m really passionate about women’s rights and women’s empowerment,” she says. “And so my entry into global health was around maternal health.”
Ratcliffe returned to school and received a master’s in Global Health and Population with a concentration in Maternal and Child Health from the Harvard T.H. Chan School of Public Health. She’s now the Assistant Director of Research on the Primary Health Care team at Ariadne Labs.
In her role, Ratcliffe has been deeply involved in the Primary Health Care Performance Initiative (PHCPI), a partnership of country policymakers, health systems managers, advocates, and others who are passionate about catalyzing primary health care improvements in low- and middle-income countries. PHCPI was founded in 2015 by the Bill & Melinda Gates Foundation, the World Health Organization, and the World Bank Group, in collaboration with Ariadne Labs and Results for Development.
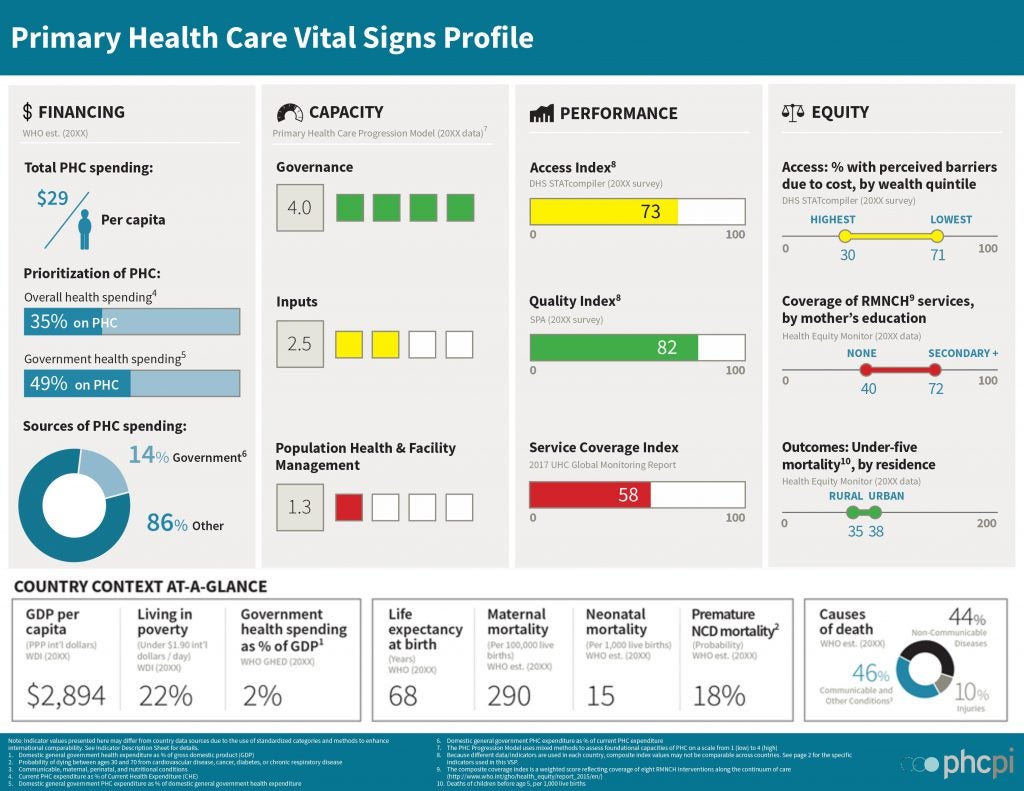
Ratcliffe’s role at Ariadne includes designing and working with countries to scale implementation of the Primary Health Care Progression Model, a mixed-methods assessment tool created by PHCPI for measuring the foundational capacities of primary health care systems—factors including governance, leadership, and population health management. The Primary Health Care Progression Model utilizes the wealth of information, evidence, and data that is often available in countries but rarely captured in a way that generates usable information for decision makers or external audiences.
Information gathered for a Progression Model can then be used to create a Vital Signs Profile. “A Vital Signs Profile is in essence a snapshot of how a country’s primary health care system is performing,” Ratcliffe says. “The idea is we can provide a one-page picture at a high level of what is going on with a primary health care system. It’s a way for different departments within ministries to engage with each other and development partners to create a common understanding of what the baseline is and where the areas for improvement are.” With support from PHCPI, five diverse “trailblazer” countries—Argentina, Ghana, Rwanda, Senegal, and Tanzania—have completed a Vital Signs Profile, and dozens more countries are in the process of completing theirs.
We caught up with Ratcliffe just after she returned from a PHCPI Training and Partner Country Workshop in Nairobi, Kenya. The workshop brought together senior policymakers and technical staff from more than 20 countries as well as representatives from global organizations such as UNICEF and the Global Fund. They shared findings and lessons learned from engagements with PHCPI and discussed ways to improve primary health care.
How was the Nairobi conference?
It was fantastic. We had 75 people from 20 countries. Primary health care is increasingly in the global spotlight, with the realization that primary health care is the cornerstone of a country’s overall health system. Our conversations at these conferences have fundamentally shifted. Three years ago it was: “Why should I do a Vital Signs profile? Why does this matter?” The question now is: “How do I do this and how do I do it well?” I think maybe one of the real indicators of success for this meeting was that at the end of four very long days the room was still full. The excitement and the engagement were really amazing. One participant said, “This is magic. You’ve fundamentally changed the way we talk about primary health care in Rwanda.”
Were there any common problems that everybody seemed to have?
There were several. Most countries lack data. So the challenge of putting together a Vital Signs Profile is identifying the data that you do have. Also, the Vital Signs Profiles are at a national level, so a common need was to be able to apply these tools to subnational levels, regions, and districts to get more nuanced pictures. And then there’s the question: What the heck do I do next?
Exactly. How does a Vital Signs Profile actually lead to improvements?
Measurement is not an end. It’s just a means to an end. We have created an Improvement Strategies section on the PHCPI website on where you can find examples of best practices and case studies of countries that have improved primary care. For example, the section on improving access to primary care has detailed case studies from Thailand, Afghanistan, and Mongolia. The Improvement Strategies are really a massive amount of work—at times it has felt like the team has tried to boil the ocean across all these different content areas.
Boil the ocean? What does that mean?
(Laughing) It’s not quite boiling the ocean but there’s so much evidence out there about primary health care and it exists in different places: peer-reviewed literature, white papers, in people’s brains. We have tried to examine everything that’s out there for a particular topic and included what’s most valuable on the Improvement Strategies site. By the end of the year we’ll have 13 Improvement Strategies modules on the website, each one a master’s thesis in and of itself. So it’s really incredible amount of work of really digging deep, finding the evidence, synthesizing the evidence, and, most importantly, relating it back to the Vital Signs Profiles. Countries can then access this material for implementing changes or developing solutions.
Overall, why is the Progression Model such an important tool?
The Progression Model is a novel approach to a long-standing issue. In the past, the inability to fully measure primary health care capacity has severely curtailed countries’ abilities to develop a holistic understanding of their system’s strengths and weaknesses. This in turn makes it difficult for countries to identify and implement needed improvements. The Progression Model is a new way of measurement and for the first time allows us to systematically measure things people know are critical for primary health care performance but had never really been measured in a standardized way.
The research conducted by Ariadne’s Primary Health Care team seeks to create a clear language around what primary health care is and develop an appropriate set of measures for assessing primary health care that can be adapted globally. Visit our site’s Primary Health Care section for information on the five key functions of primary health care and links to our primary health care research.
—Interview conducted by Stephanie Schorow


